The Development and Mechanisms of Capnography for Anesthesia
Capnography, the non-invasive measurement of carbon dioxide (CO2) concentration in exhaled breath, is an invaluable tool in the field of anesthesia. Its evolution and integration into anesthetic practices have significantly enhanced patient safety and the precision of care delivery. In this article, we delve into the development of capnography and its mechanisms, particularly in the context of anesthesia.
Historical Context and Development
The journey of capnography began in the 20th century when CO2 was identified as a critical component to monitor during anesthesia. However, the technology to measure CO2 accurately and continuously was lacking until the latter half of the century. The initial methods were rudimentary, relying on colorimetric techniques that lacked precision.
It wasn’t until the 1970s that mainstream capnography emerged, thanks to the development of infrared spectroscopy technology. This method, based on the principle that CO2 molecules absorb infrared light at a specific wavelength, allowed for continuous and accurate measurement of exhaled CO2. Its integration into clinical practice was gradual, with the recognition of its potential to prevent anesthesia-related complications. By the late 1980s, capnography had become a standard monitoring tool during general anesthesia.
Principles and Mechanisms
At its core, capnography measures the partial pressure or concentration of CO2 in the respiratory gases. This is achieved through the mainstay technology of infrared absorption. CO2 has a characteristic absorption spectrum in the infrared range, and the amount of light absorbed is directly proportional to the concentration of CO2 in the sample. Modern capnographs utilize this principle, shining an infrared light through a sample of exhaled gas and measuring the amount of light absorbed.
The resultant waveform, known as a capnogram, provides real-time information about the patient’s ventilatory status. A typical capnogram consists of four phases:
- Baseline (Phase I): Represents inspired gas, which is normally devoid of CO2.Expiratory Upstroke (Phase II): Reflects the rapid rise in CO2 as alveolar gas is exhaled.
- Alveolar Plateau (Phase III): Indicates the CO2 level in alveolar gas, crucial for assessing ventilation.
- Inspiratory Downstroke (Phase 0): The drop in CO2 concentration as inhalation begins.
Capnography in Anesthesia
In the realm of anesthesia, capnography serves several critical functions:
- Verification of Endotracheal Tube Placement: The presence of a capnographic waveform immediately after intubation confirms that the endotracheal tube is in the trachea and not the esophagus.
- Monitoring Ventilation: Continuous capnography allows anesthetists to monitor the adequacy of ventilation and make timely adjustments to ventilator settings. It is especially crucial during long surgeries and when muscle relaxants are used.
- Early Detection of Respiratory Complications: Capnography can detect hypoventilation, airway obstruction, accidental extubation, and equipment failure long before hypoxemia becomes evident on pulse oximetry.
- Assessment of Circulatory Status: Sudden changes in the capnogram can indicate circulatory failure, pulmonary embolism, or cardiac arrest, prompting immediate intervention.
- Weaning from Mechanical Ventilation: Capnography aids in assessing readiness for extubation and monitoring for hypoventilation in the postoperative period.
Innovation and Future Directions
The continued development of capnography technology focuses on enhancing accuracy, minimizing response time, and integrating capnographs with other monitoring systems. Newer designs aim to make the devices more compact, portable, and user-friendly, expanding their use beyond operating rooms to intensive care units, emergency departments, and pre-hospital settings.
Research is also exploring the use of capnography in non-intubated patients, pain management, and sedation practices. There’s an increasing interest in capnography’s role in monitoring breathing patterns, providing insights into respiratory pathophysiology.
Conclusion
The development of capnography represents a remarkable leap in patient safety and care during anesthesia. Its real-time monitoring capabilities have fundamentally changed how anesthesiologists manage ventilation and detect complications. As technology advances, capnography will continue to evolve, further cementing its role as an indispensable tool in modern anesthesia practice.
More From The Blog
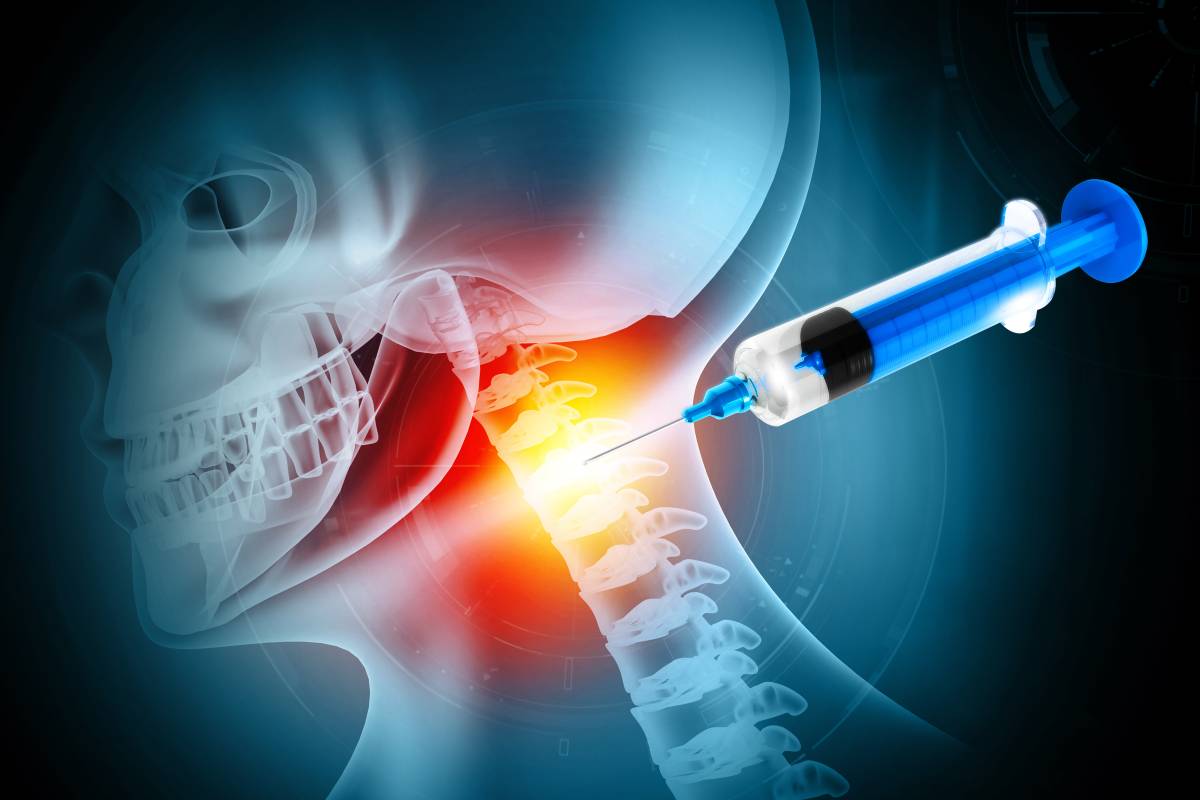
Neuraxial Anesthesia in the Cervical Spine
Neuraxial anesthesia, encompassing both spinal and epidural anesthesia, is typically reserved for surgeries involving the lower abdomen, pelvis, and lower extremities to avoid impairment of

Propofol in Anesthesia: Uses and Mechanism
Propofol is a widely used anesthetic agent known for its rapid onset and short duration of action. It plays a crucial role in modern anesthesia