Reasons Against Using Remimazolam As An Anesthetic Agent
Remimazolam, a newer intravenous anesthetic agent, has gained attention in the medical community due to its unique pharmacological properties, such as rapid onset and short duration of action. As a benzodiazepine derivative, it provides sedation and anxiolysis, with a primary use in procedural sedation and general anesthesia. Despite these promising features, there are several reasons why remimazolam may not be an ideal choice for every clinical situation, and anesthesiologists may decide against its use in favor of other anesthetic agents like propofol, midazolam, and thiopental. Understanding these drawbacks is essential for making informed decisions in anesthesia practice.
Given its relatively recent approval, one significant concern with remimazolam is the lack of extensive long-term clinical data. Although the agent has shown efficacy in shorter procedures and has been well-received in specific settings, there remains a paucity of evidence regarding its long-term safety, particularly in critically ill patients or those with chronic health conditions. This lack of data means that its safety profile over extended periods or repeated exposures is not fully understood. Additionally, the pharmacokinetics in different patient populations, such as those with liver or renal dysfunction, have not been as thoroughly explored as with older agents, which raises concerns about its use in these groups.
Another limitation of the use of remimazolam is its cost. It is relatively expensive compared to more commonly used agents like propofol or midazolam. This financial barrier may make its routine use less feasible in settings where cost-effectiveness is a major consideration, such as in public health systems or for patients without substantial insurance coverage. The high cost may be sufficient reason to decide against using remimazolam in many standard procedures, especially when more established and equally effective alternatives are available at a fraction of the price.
Furthermore, remimazolam’s pharmacodynamics, though advantageous in some respects, can be a disadvantage in others. While it provides rapid induction and quick recovery, the short duration of action is not ideal for longer procedures. In cases where a prolonged sedative effect is necessary, it may require repeated dosing, which could increase the risk of accumulation and side effects. Additionally, the need for frequent administration may reduce the overall convenience of the agent, particularly in settings where continuous monitoring and dose adjustments are not always feasible. In longer procedures, anesthesiologists continue to opt for other drugs.
There are also concerns related to the cardiovascular stability of remimazolam. Like other benzodiazepines, it can cause hypotension and respiratory depression, which are often dose dependent. Although these effects may be less pronounced than with other agents, they still pose a risk, especially in patients with compromised cardiovascular function. Given that remimazolam is often used in sedation for procedures that may not warrant the intensive monitoring required in a general anesthetic setting, these cardiovascular concerns can be exacerbated in patients who are hemodynamically unstable or those undergoing more invasive procedures.
Healthcare providers should also consider the potential for drug interactions when using remimazolam. Although the agent is metabolized by esterases, which could theoretically limit interactions with cytochrome P450 enzymes, the full spectrum of possible drug interactions is not yet completely characterized. In polypharmacy patients, such as those receiving treatment for comorbid conditions, the risk of unforeseen interactions remains a valid concern. This is particularly relevant in patients who are on medications for hypertension, epilepsy, or other chronic diseases that may influence drug metabolism or cardiovascular status.
Finally, the lack of user familiarity and clinical experience with remimazolam may present issues. While remimazolam’s use is growing, many anesthesiologists and sedation practitioners are far more experienced with agents like propofol, midazolam, or ketamine, all of which have a well-established safety and efficacy profile. This comfort level with traditional drugs is a significant reason that some practitioners may be against adopting a newer agent like remimazolam, especially if they perceive it as less predictable or insufficiently proven.
In conclusion, while remimazolam offers a novel approach to sedation and anesthesia with many advantageous properties, there are several reasons to consider against its use, depending on the clinical scenario. These reasons include limited long-term safety data, higher costs, the potential for increased dosing in longer procedures, cardiovascular concerns, drug interactions, and limited practitioner experience. Given these issues, it is essential for healthcare professionals to weigh the benefits and drawbacks of remimazolam carefully, considering the individual patient’s needs, the procedural requirements, and the available alternatives.
More From The Blog
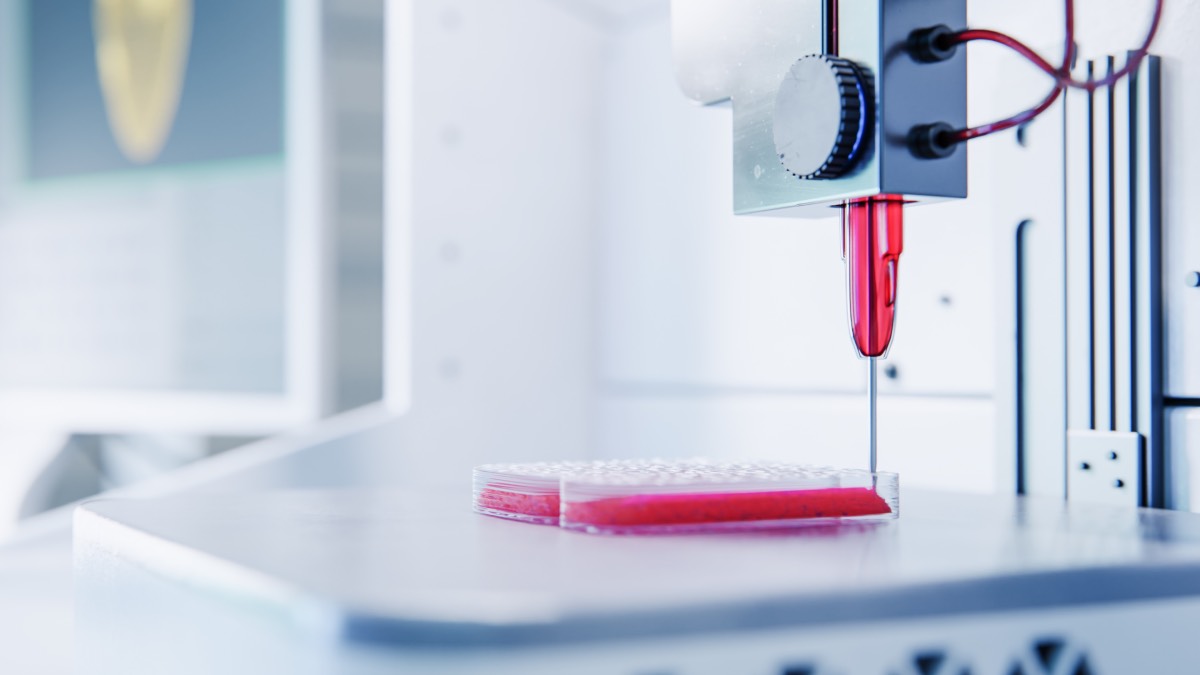
Bioprinting for Medicine
Bioprinting is an emerging medical technology that often captures public imagination, but it is important to understand both its promises and its present limitations. At

Virtual Reality for Anesthesia Training and Education
Virtual reality is a powerful tool for anesthesia training and education, offering new ways for trainees to practice complex skills in a safe and controlled